Why Mental Health Should be Addressed by All Doctors in Primary Health Care
In 1948, the constitution of World Health Organization (WHO) recognized health to have two crucial dimensions- physical and mental. Since then, as stated in the definition, health is considered as ‘a state of complete physical, mental and social well being and not merely the absence of disease or infirmity’. This definition highlights two important aspects of health- (i) health is not merely the absence of diseases but a state of well being as well and, (ii) health is not just the state of physical well being but the mental and social well being as well.
 It must be understood that mental health care is as ‘primary’ as physical health care. Primary care for mental health refers specifically to mental health services that are integrated into general health care at a primary care level. Primary care for mental health pertains to all diagnosable mental disorders, as well as to mental health issues that affect physical and mental well-being
It must be understood that mental health care is as ‘primary’ as physical health care. Primary care for mental health refers specifically to mental health services that are integrated into general health care at a primary care level. Primary care for mental health pertains to all diagnosable mental disorders, as well as to mental health issues that affect physical and mental well-being
This article reviews the need solely, from an Indian perspective. There are several statistics revealed that highlight the alarming need for increasing, improvising and integrating mental health care into the primary health care ecosystem.
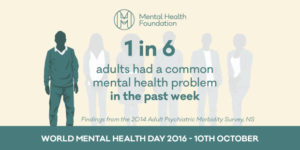
Mental disorders are extremely prevalent in all countries and are responsible for immense suffering, poor quality of life, increased mortality and staggering economic and social costs. The number of people suffering from mental illnesses in India alone exceeds the population of South Africa. At present, people suffering from mental illnesses account for nearly 6.5 percent of the country’s population and it is estimated that by 2020, this number will increase to a staggering 20 percent. One in every 22 people suffers from depression, suicide rates are distressingly increasing among the younger age range of 15-29 years and more than 60 million people suffer from some form of common or severe mental health disorder. Mental illnesses cannot continue to be ignored and rather, demand for a system which respects human rights and promotes good health outcomes and recovery through the delivery of mental health care in the primary health-care system.
The rates at which the stigma against mental health is dissolving, especially in India, is decelerated. With the growing burden of mental health issues on the people of the nation, the stigma attached to these illnesses continues to prevail and abstains people from receiving the required treatment. Several other factors like lack of trained professional help, treatment gap and impeded awareness- widen the gap between illness and care. The scenario calls for a collective functioning of the health ecosystem in order to fill in this gap and reduce the burden of illnesses on a national (and global) level.
When mental health care is integrated into primary health care, it involves several other parties such as governmental and non-governmental bodies, local bodies, institutions at the village, community and urban levels along with the involvement of physicians and mental health professionals. Responsibility for public health care in India lies with the national and state governments. Health care is provided at a number of different levels. Two significant developments heralded the integration of mental health into primary care in India: the launch of the National Mental Health Programme in 1982, and the revision of the National Health Policy, which specified the inclusion of mental health in general health services, in 2002. In India, at the policy level, the National Mental Health Programme (NMHP, 1982), District Mental Health Programme (DMHP, 1995) and the recently passed Mental Health Care Bill (2016-17) re-emphasize for the consolidated services in the existing healthcare paradigm.
It is important to emphasize that mental health care delivered in this setting is much more likely to be effective and long-lasting if complemented by a strong secondary level of care to which primary health care workers can turn to for referrals, as well as for support and supervision. Having in place strong informal community mental health services and support groups, run by NGOs and faith-based organizations can also complement and strengthen the services provided through primary healthcare services.

The district of Thiruvananthapuram in Kerala (India) is a classic case demonstration of the integrated services of mental health within primary health care that has been operational since 1999. Trained medical officers diagnose and treat mental disorders as part of their general primary care functions. A multidisciplinary district mental health team provides outreach clinical services, including direct management of complex cases and in-service training and support of primary care workers. The free and ready availability of psychotropic medications in the clinics has enabled patients to receive treatment in their communities, thus greatly reducing expenses and time spent traveling to hospitals.
The benefits of integrating mental health into primary healthcare are significant. On one hand, integration ensures that the population as a whole has smoother access to the mental health care that they need early in the course of disorders. On the other hand, when people receive treatment in primary healthcare facilities the likelihood of better health outcomes, and even full recovery, as well as maintained social integration is increased.
Other reasons for such integration include:
1. The burden of mental disorders is huge and needs quick attention.
2. Mental and physical health problems are interwoven and affect each other.
3. The treatment gap for mental disorders is enormous and this integration will help reduce this gap.
4. Primary care for mental health increases and eases access to mental health services.
5. Primary care for mental health promotes respect of human rights (every person suffering from a mental illness has the right to get treatment at the right time).
6. Primary care for mental health is affordable and cost-effective.
7. Primary care for mental health generates good health outcomes.
8. In a country like India, where the number of mental health professionals is insufficient, a consolidated primary health care system makes an available larger number of professionals responsible for early intervention and treatment.
The reason we need mental health services in primary health care is also that it is seen that people frequent the primary health care practitioners with greater ease and report problems that come under the mental health problems umbrella. As research has found out, the prevalence of mental disorders in primary care settings has been present extensively in a range of different countries. Among adults, the principal mental disorders presenting in primary care settings are found to be- depression, generalized anxiety disorder, substance use and dependence, and somatization disorders. Studies of children and adolescents have also demonstrated a high prevalence of mental disorders in primary care settings, with the most common diagnoses as anxiety disorders, major depression, conduct disorders and attention-deficit/ hyperactivity disorder. Among elderly people in primary care, the prevalence of mental disorders can be as high as 33%, with the most common diagnoses are depression and dementia.
Mental health scenario in India has been an increasingly progressive phenomenon. The coming years are expected to be more promising with a step forward towards a consolidated primary health care paradigm providing mental health services.
For more information about options of online therapy check here
This Article is being republished with the permission of the Author from TBI.
About the Author:

Pragya Lodha is the Assistant Editor of the Indian Journal of Mental Health and works as a Research Assistant at De Sousa Foundation, Mumbai with over 20 publications in National and International publications in journals and books. Pragya has been working in the field of mental health, engaging in various on the ground and online projects. She also serves as the Associate Programme Developer at The MINDS Foundation, Gujarat. Presently, she is also the India Coordinator and Leader for an Indian-European Project called “Advocacy for Mental Health: Create Leaders to Innovate and Break Stigma”. She is also a Trained Volunteer at Samaritans Mumbai for 2 years with a background in Clinical Psychology and Psychotherapy. Pragya aspires to see mental health as a comfortably spoken about and addressed domain in India, in the coming time.

Leave a Reply